Using Falck Medical Tonography to Confirm the Effectiveness of Outflow Therapy
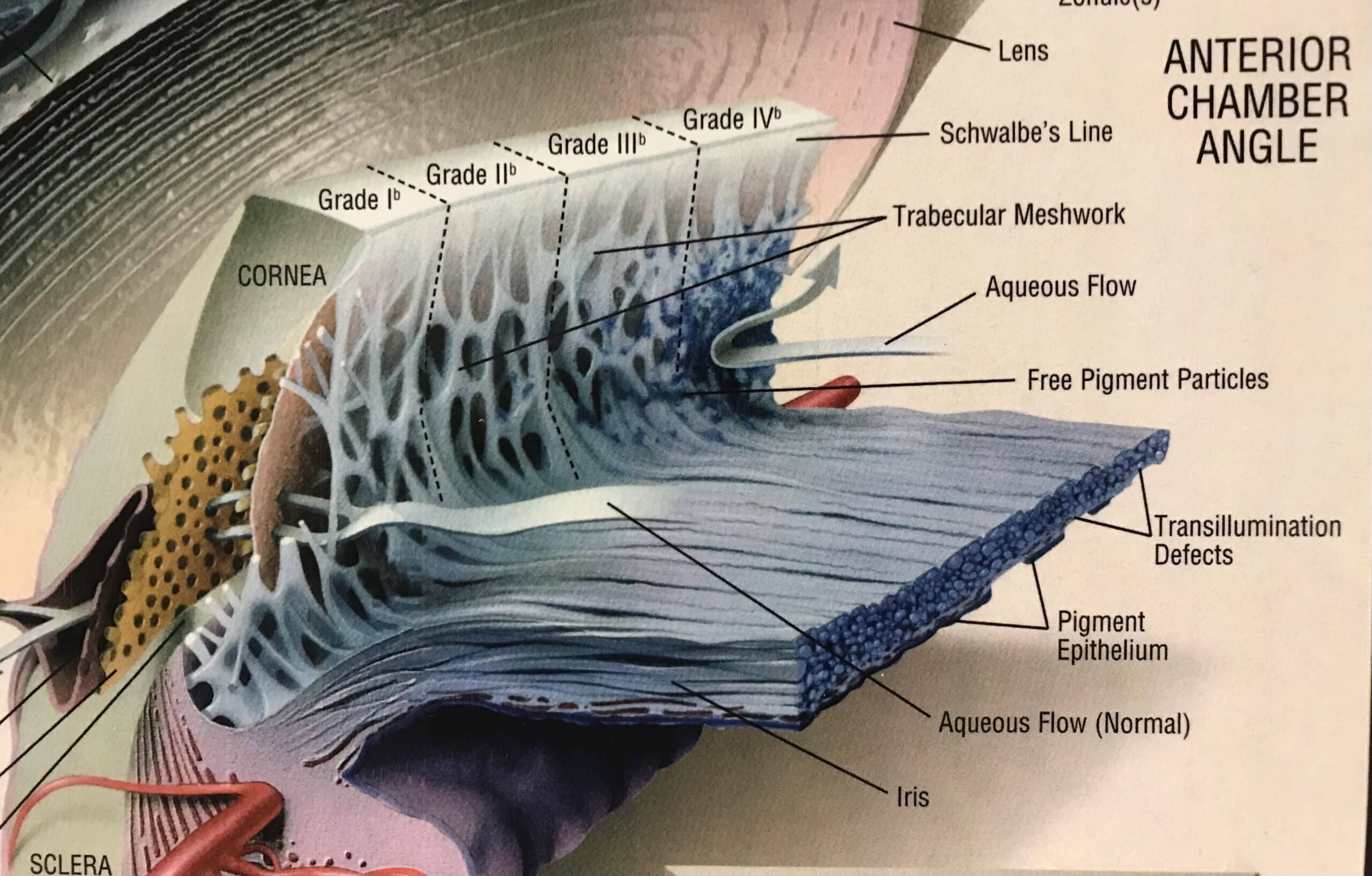
Tonography is the non-invasive measurement of aqueous humor outflow. With traditional tonography indentation force is applied to the eye to drive aqueous humor out of the eye through the trabecular meshwork. This procedure indents Descemet’s membrane and ocular distention occurs. Scleral rigidity and pseudofacility are measurement errors that occur with indentation tonography (1). If the trabecular meshwork is diseased, outflow is impaired. In both open angle and closed angle glaucoma aqueous humor outflow is impaired. If outflow is impaired, the intraocular pressure (IOP) can increase to abnormal levels (2). IOP is directly proportional to aqueous humor production, measured in µL/min, and inversely proportional to aqueous humor outflow, measured in µL/min/mmHg, as shown below.
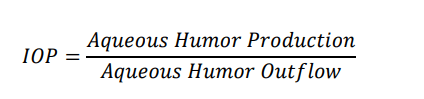
IOP is not static, it varies significantly throughout the day due to changes in aqueous humor production by the ciliary body. In eyes with impaired aqueous humor outflow, the magnitude of IOP variation is much greater (2,4). Intraocular pressure measured in the office is not equivalent to the IOP outside the office. Intraocular pressure outside the office will likely be higher. It is only highest in the morning when aqueous humor production increases dramatically. When aqueous humor production increases and aqueous humor outflow is impaired, the IOP will increase to damaging levels (3,4). Because of this significant variation of IOP, the measurement of IOP may only have clinical value if it is checked multiple times during a twenty-four hour period (4). In contrast to varying aqueous humor production, aqueous humor outflow is relatively constant. Measuring aqueous humor outflow in the office can predict IOP outside the office. Setting a target outflow facility value can control the IOP variation outside the office (4,5).
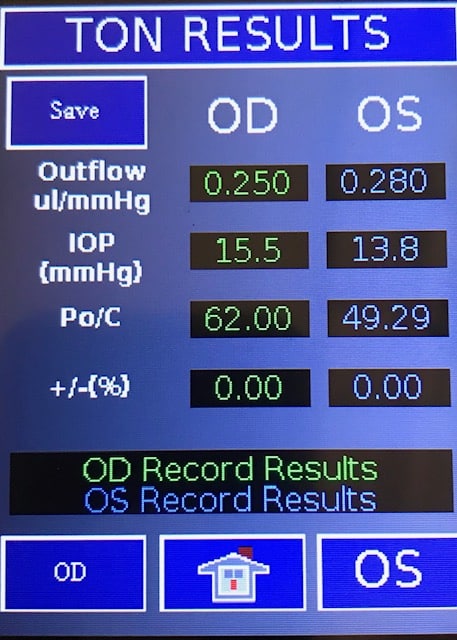
The Falck Medical, Inc FMD tonography (TNG) measurement is the first and only aqueous humor outflow procedure cleared for clinical use by the United States Food and Drug Administration (USFDA) (5). The FMD tonography procedure uses the applanation method. Descemet’s membrane is not indented. Measurement errors related scleral rigidity and pseudofacility are reduced. In the USFDA CRO Pre IDE tonography research study, the severity of glaucoma was directly correlated with the severity of impaired outflow. One hundred ninety-two eyes were enrolled. In eyes with advanced stage glaucoma, outflow was less than 0.09 ul/min/mmHg, moderate stage glaucoma 0.10 to <0.16 ul/min/mmHg and mild stage glaucoma 0.16 to 0.18 ul/min/mmHg (p < 0.05). Additional information obtained from this study was the relationship between IOP variation and impaired aqueous humor outflow. In eyes with outflow <0.10 ul/min/mmHg the IOP increased to an average of 35 mmHg (r2 = 0.88). All eyes with glaucoma had outflow values less than 0.18 ul/min/mmHg. The difference in outflow between eyes with glaucoma and eyes without glaucoma was statistically significant different, p = <0.0001. All patients with glaucoma had an IOP/Outflow Facility Ratio (Po/C) greater than 100 (5). This is consistent with the work of Grant et al who found that 95% of eyes with a Po/C ratio greater than 100 had glaucoma (4). It is well known that IOP is not static and the in office IOP does not correlate with IOP outside the office. It is also established that in eyes with open angle and closed angle glaucoma aqueous humor outflow is impaired. It has also been confirmed that in office measurement of outflow facility (TNG) can be used to manage and control IOP outside the office (4). All current prostaglandin eye drop therapy is directed at improving outflow facility. Laser trabeculoplasty, MIGS, Trabeculectomy, Goniotomy and Seton procedures are also directed at improving outflow of aqueous humor. Measuring IOP alone cannot confirm the effectiveness of outflow therapy. The underlying natural variation of IOP can give the false impression that the outflow therapy has been effective.
The only way to confirm the effectiveness of outflow therapy, is to measure outflow. The major benefit of tonography is confirming the clinical effectiveness of outflow therapy. To properly manage glaucoma, which is a disease of impaired aqueous outflow, tonography must be used to evaluate the effectiveness of outflow therapy and control the damaging elevation of IOP
References:
1.Manual of Tonography. Robert C. Drews. 1971. C. V. Mosby Company.
2. Adlers Physiology of the Eye. 10th Edition. Kaufman P, et al Aqueous Humor Dynamics. Pages 238-239.
3. The Glaucomas. Volume 1. 1989. Ritch R, et al. Tonography. Pages 296-297.
4. Chandler and Grants Glaucoma. Fourth Edition. 1997. Epstein DL, et al. Tonography. Pages 47-50.
5. United States Food and Drug Administration CRO Pre-IDE 510k151491 Tonography
